
- O nas
- Dystrybutorzy
- Formularz
 Polski
PolskiChoisissez votre langue Scegliete la vostra lingua Wählen Sie Ihre Sprache Escolha o seu idioma ??????????? ?????? Choose your language
Menu

Photoactivated chromophore for keratitis?corneal cross-linking or PACK-CXL is one of the most exciting aspects of CXL today. But there are still some misconceptions about it: treating infectious keratitis with CXL is not like treating keratoconus with CXL. A recently published clinical trial in Ophthalmology (1), plus a letter published in response (2) highlighted this.
Prajna et al. (1) used PACK-CXL to treat fungal keratitis. In their study, 111 patients received either topical antifungal drugs (either natamycin 5% or amphotericin 0.15%) with or without PACK-CXL. They concluded that “there appears to be no benefit of adjuvant CXL in the primary treatment of moderate filamentous fungal ulcers, and it may result in decreased visual acuity”.
However, Hafezi et al. (2) believe that there was a fundamental flaw in their trial design that resulted in an insufficient amount of UV irradiation (fluence) being used to treat fungal infections during PACK-CXL.
The publication had several flaws. Basic details were missing such as the baseline ulcer size and the UV fluence that was applied. However, the methods section cited the ?Dresden Protocol? (3), the classic method of performing cross-linking in corneas with keratoconus. This involves 30 minutes 0.1% riboflavin instillation, followed by 30 minutes of 3 mW UV illumination, for a total fluence of 5.4J/cm². We could therefore assume that the Dresden Protocol was used to treat patients in the clinical trial.
The Dresden protocol is inadequate for the treatment of infectious keratitis, regardless of whether it is bacterial or fungal in origin. To explain why, we need to examine what happens with corneal cross-linking.
When a riboflavin-saturated stroma is hit by a photon of UV light, the riboflavin is activated, reacts and generates reactive oxygen species (ROS), which can cross-link the molecules of the stroma with one another, or damage the cell membranes and nucleic acids of pathogens. It is a challenge for the UV light to penetrate much deeper as riboflavin also acts as a protective shield (although once UV-activated-riboflavin has reacted with other molecules, it is consumed and can no longer absorb UV energy). To penetrate deeper needs more UV energy to be delivered.
Riboflavin acting as a shield against UV energy is good in many ways, as it protects the corneal endothelial cells at the base of the cornea from damage from UV radiation. But it also means that the UV energy absorption decays in a logarithmic manner. The amount of UV energy delivered by the Dresden Protocol therefore only cross-links the first 100 µm.
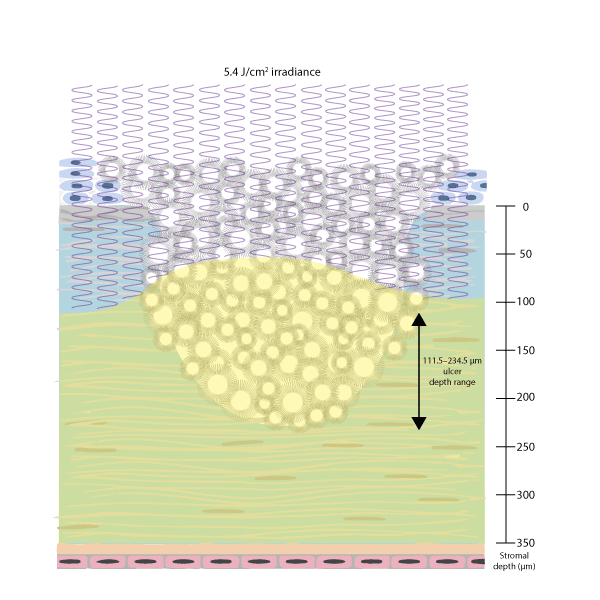
So how deep were the ulcers in these patients? The Methods section states that eyes with ?involvement of the posterior one-third of the stroma? and ?central pachymetry less than 350 mm? were excluded, and that 46% and 68% of patients treated with CXL (natamycin and amphotericin, respectively) had ulcer depths of 33-67% of the depth of the stroma.
Let’s do a little math to find the lowest possible ulcer depth (and therefore the best chance of successful treatment with a PACK-CXL protocol, in which only the top 100 µm of the cornea are treated).
If the thinnest cornea in the study was 350 µm and the shallowest ulcer depth range was 33?67%, this means that the ulcer depths are in the range of 111.5?234.5 µm ? and thus thicker corneas would have even deeper ulcers.
But these assumptions are all being made that the cornea is a keratoconic and not ulcerated. Corneal ulcers are opaque, meaning that it is even more difficult for UV light to penetrate the cornea. All in all, this means that even in the best-case scenario, insufficient UV energy is being delivered to the cornea to treat all of the infection.
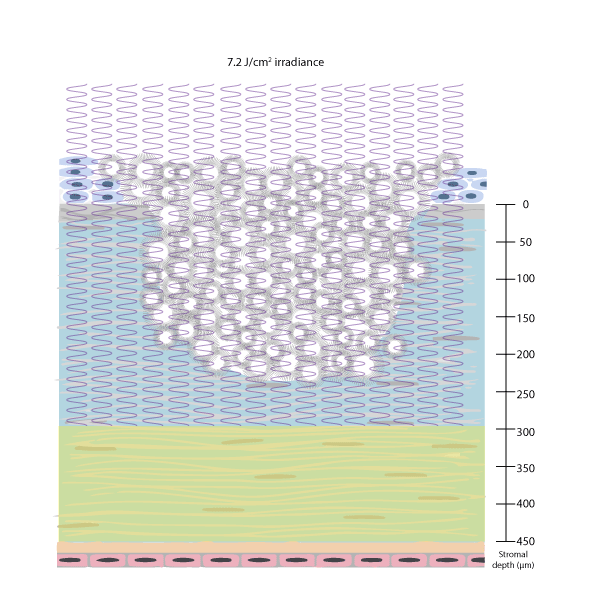
Hafezi et al. (2) noted that they have already shown that PACK-CXL is more effective at killing bacteria when higher UV fluences are used (4), and state that in their ongoing clinical study, the effectiveness of PACK-CXL with a total fluence of 7.2 J / cm² is similar to antimicrobial therapy.
You need to deliver more energy than traditional keratoconus cross-linking methods to ensure that the effect is deep enough to treat deep ulcers.
References